Therapeutic Role of Yoga in Neuropsychological Disorders
Authored by: Elnaz Nourollahimoghadam, Shaghayegh Gorji, Ali Gorji, Maryam Khaleghi Ghadiri
Abstract
Yoga is considered a widely used approach for health conservation and can be adopted as a treatment modality for a plethora of medical conditions, including neurological and psychological disorders. Hence, we reviewed relevant articles entailing various neurological and psychological disorders and gathered data on how yoga exerts positive impacts on patients with a diverse range of disorders, including its modulatory effects on brain bioelectrical activities, neurotransmitters, and synaptic plasticity. The role of yoga practice as an element of the treatment of several neuropsychological diseases was evaluated based on these findings.
Core Tip
A multitude of beneficial effects of yoga practice and the underlying mechanisms of action have been reported and point out its role as an influential element in the integrative therapy of various neuropsychological disorders. In the planning of further investigations, studies should be designed to achieve more accuracy and precision in the heterogeneous field of yoga practices and potential fields of application.
Introduction
Several neurological disorders affect mental health and lead to various degrees of impairment in cognitive functions. The use of complementary and alternative medicine, practices that improve the mind’s capacity and body function, amongst patients with neuropsychological disorders is increasing worldwide [1,2]. Biofeedback, homeopathy, acupuncture, meditation, and yoga are among the different categories of these interventions [3]. Yoga is a form of mind-body technique that involves and contributes to both mind and body [4] and has been used as a therapeutic intervention in various neurological and psychological disorders [5]. The word “Yoga” is derived from the Sanskrit origin “yuj” meaning “yoke” or “union,” and it is assumed that yoga describes the union between mind and body [5]. As an ancient Indian non-religious mind-body method [2,6], yoga is considered a philosophical and spiritual discipline that alleviates suffering and promotes human health [4]. Yoga has been practiced in Eastern cultures as a spiritual healing method for over 4000 years. The “Yoga sutra,” a 2000-year-old guidebook, is the earliest known document of yoga that provides the framework of all branches of yoga. This book conceptualized yoga as eight limbs, which were designed to be practiced in sequence [7-9].
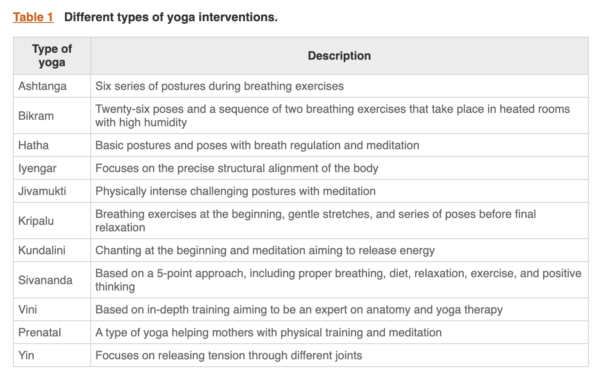
There are several styles of yoga, and no one is superior to another (Table 1). Table 1
A rapid increase of interest in yoga in Western countries occurred in the first decades of the 19th century, which has continued to this day. The National Health Interview Survey has reported that the number of people in the United States who practice yoga has increased dramatically among all age groups between 2002 to 2012[9,10]. Yoga practice can be a treatment for a variety of disorders as well as physical exercise [9]. This leads to an increase in investigations focusing on the mechanism of action and effect of yoga intervention on various mental and physical conditions [9-11]. Yoga interventions can maintain brain health through various mechanisms, such as the improvement of cerebral oxygenation [12], enhancement of neurotrophic and angiogenic factors (such as angiogenin) [13], balancing the excitatory/inhibitory neurotransmitter equilibrium [14], modulation of immune responses [15], and prevention of oxidative stress [16].
In the present review, we first show data that point out the effect of yoga on the brain under physiological conditions. Then, we review the effect and potential mechanism of action of yoga in the treatment of neurological and psychological disorders.
EFFECT OF YOGA ON THE BRAIN
Yoga is a movement-based embodied contemplative activity that can lead to a variety of neurobiological alterations in different brain regions. Yoga exerts a regulatory effect on brain synaptic plasticity and promotes cognitive tasks, particularly working memory [17,18]. Furthermore, yoga increases inter-hemispheric coherence and symmetry and improves neurocognitive functions [19]. Yoga may also exert pronounced anatomical changes in different brain regions, especially in the limbic system [20].
The effect of yoga on brain neurotransmitters γ-aminobutyric acid (GABA) is considered the main inhibitory neurotransmitter responsible for the regulation of cortical excitability and neural plasticity [21,22]. Multiple lines of evidence suggest that yoga promotes cortical GABAergic inhibitory tone and modulates downstream brain regions [14,23]. A 12 wk yoga practice markedly enhanced the thalamic GABA values, accompanied by improved mood and reduced anxiety [24]. Higher thalamic GABA levels could be the result of enhanced (regional) cerebral blood flow in the prefrontal cortex of yoga practitioners [25], which can lead to the activation of the reticular nucleus of the thalamus and higher GABA production [26,27]. A magnetic resonance spectroscopy study has shown that yoga practitioners exhibited greater brain GABA values after a 60 min session of yoga training compared to controls [28]. In addition to GABA, an enhancement of dopamine has been observed in the ventral striatum of subjects who practice yoga [25,29,30]. It has been suggested that yoga could cause a rise in serotonin. Several investigations performed on participants after their meditation sessions have shown an elevation of the serotonin metabolite levels in urine [25,31]. Moreover, regular yoga practice may cause a reduction in norepinephrine values. Patients with heart failure who practiced weekly yoga displayed lower levels of norepinephrine in blood samples [30,32] (Figure 1).
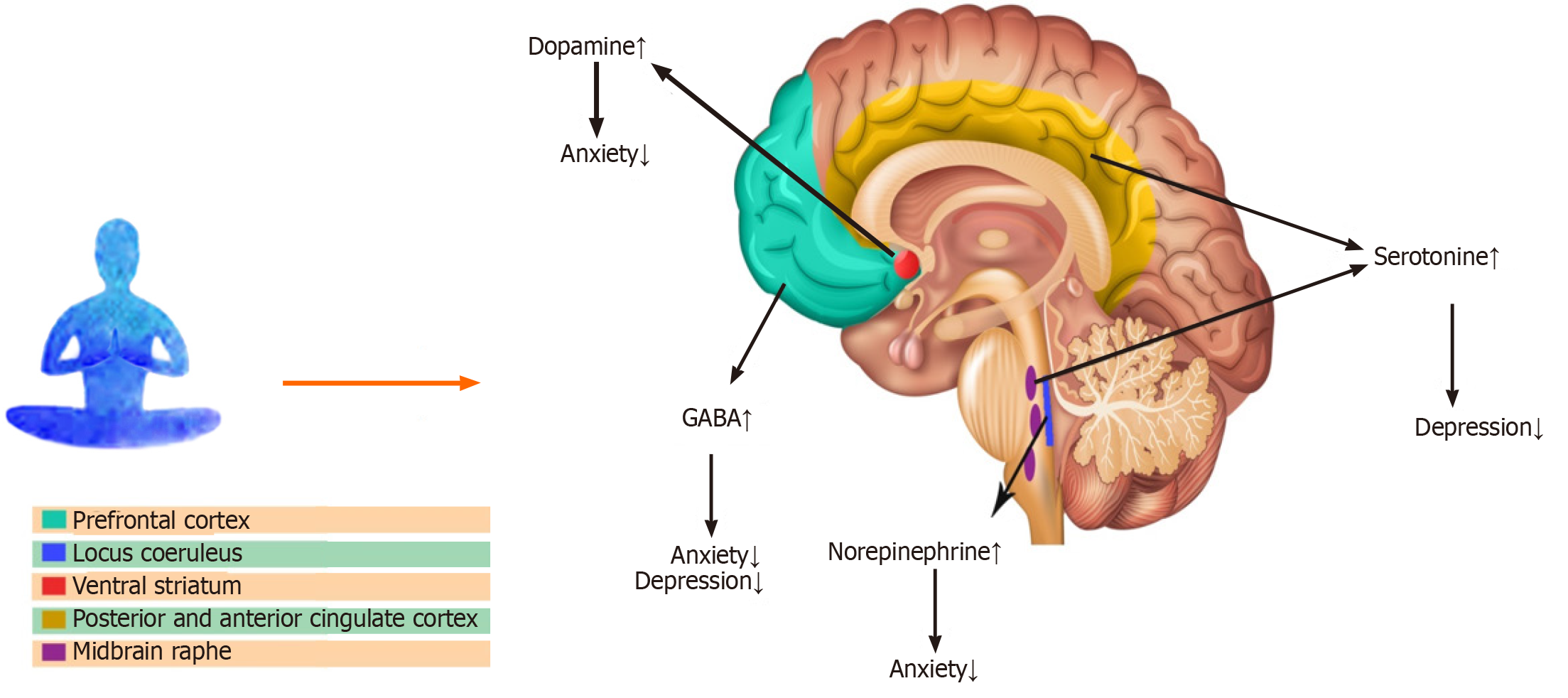
Figure 1 The effect of yoga intervention on various neurotransmitters in different brain regions. GABA: γ-aminobutyric acid.
Effect of yoga on the bioelectrical activities of the brain
Yoga practices regulate electroencephalogram (EEG) signals through switching off non-relevant neural circuits for the preservation of focused attention and blockade of inappropriate signals [33]. Studies on the effects of yoga on brain waves revealed that breathing, meditation, and posture-based yoga practice increase overall brain activity [19], particularly in the amygdala and the frontal cortex. Alpha brain waves predominate during active attention and thinking as well as in some meditative conditions and correlate with basic cognitive processes [34]. Alpha waves could reflect the physiological and pathological changes of the relevant neural network activity during conscious perception and working memory [35]. Investigations on brain waves in meditators concluded that meditation leads to alterations in anterior cingulate and dorsolateral prefrontal cortices and the enhancement of alpha wave activity [36].
Beta brain waves are dominant during wakefulness with open eyes, which could be affected by stressful conditions [37,38]. An enhancement of EEG beta wave activity has also been observed after yoga meditation practices [39]. Beta wave activity is present throughout the motor cortex during isotonic contractions and slow movements and is related to gains in academic performance and high arithmetic calculation ability [19,40]. Theta waves assist with alertness and the ability to process information quickly [36]. The occurrence of the higher theta wave activities is associated with lower levels of anxiety [36,41]. An increase in theta wave activity has been reported during meditation [30,36]. Longer duration of meditation is associated with higher theta and alpha wave activities [30,33,36].
Effect of yoga on brain structure and neural connectivity
Yoga intervention seems to be associated with brain structural alterations, particularly in the frontal cortex, amygdala, hippocampus, insula, and anterior cingulate cortex [42]. An investigation on regional differences in grey matter volume associated with the practice of yoga has shown a greater grey matter volume in different areas of the dominant hemisphere, including the ventromedial orbitofrontal, ventrolateral prefrontal, and inferior temporal and parietal cortices as well as the left insula in skilled practitioners of yoga [43]. Furthermore, elderly yoga practitioners with several years of yoga experience have shown greater neocortical thickness in the left prefrontal complex cluster, which includes part of the lateral middle frontal gyrus, dorsal superior frontal gyrus, and anterior superior frontal gyrus compared to healthy non-practitioners [44]. A magnetic resonance imaging study revealed the greater volume of gray matter in the left hippocampus in skilled yoga practitioners with at least 3 years of experience compared to the sex- and age-matched control subjects [18].
A population-based study on 3742 subjects revealed a lower right amygdala volume and a lower left hippocampus volume in those who participate in meditation and yoga practices [45] (Figure 2).
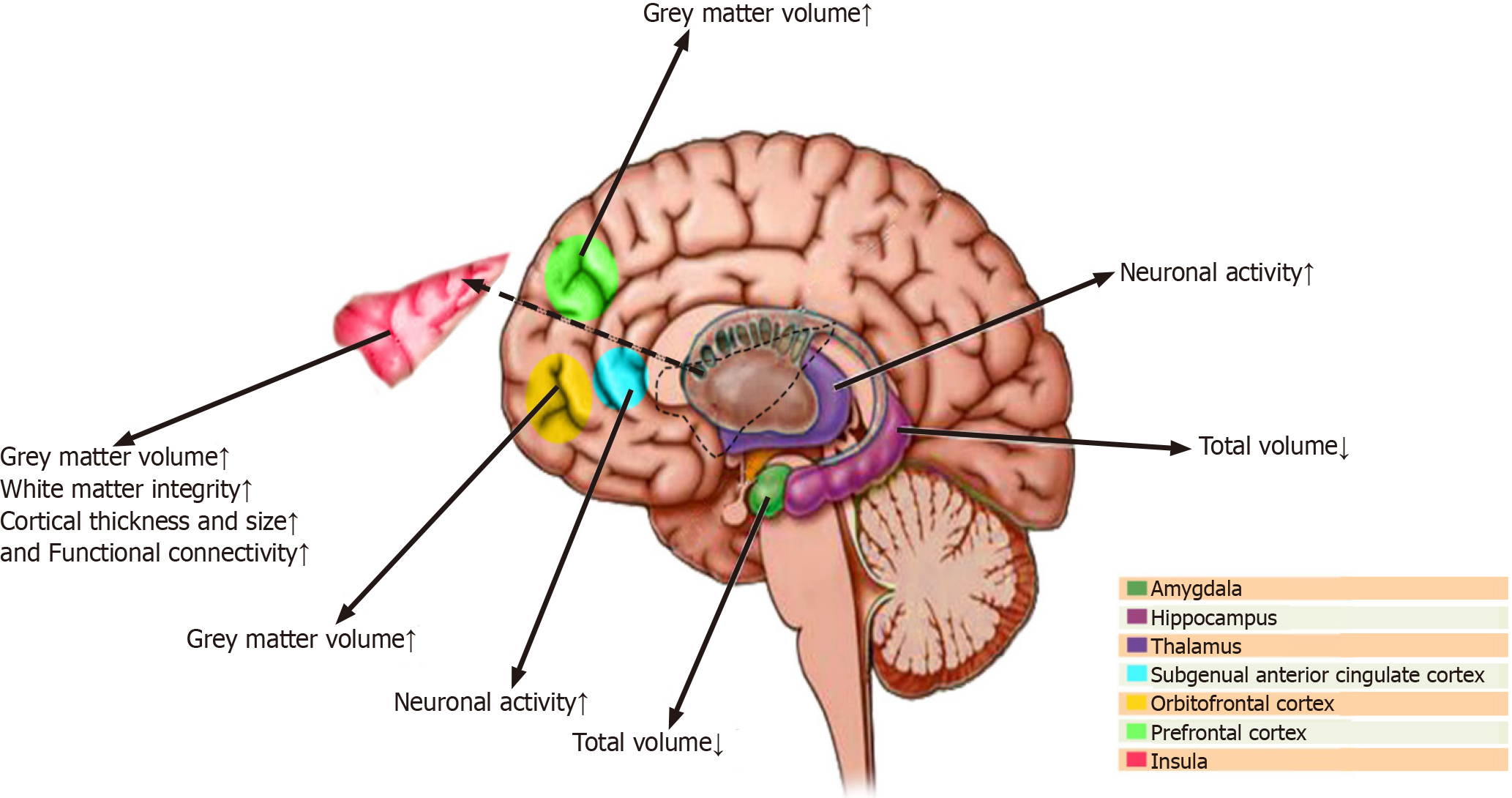
Figure 2 The effect of yoga practice on the functional activities of various brain regions.
THE CLINICAL EFFECT OF YOGA
The clinical role of yoga on neurological disorders
Yoga and headaches
Several studies have suggested the beneficial effects of yoga in reducing the frequency and intensity of various forms of headaches, particularly migraine and tension headaches [46]. Yoga has been suggested as a potential complementary therapeutic intervention for headaches [47]. A meta-analysis on yoga for tension-type headaches and migraine has shown preliminary evidence of a short-term beneficial effect of yoga on tension-type headaches. This study revealed a significant improvement in the frequency, duration, and intensity of pain in patients with tension-type headaches [48]. A randomized controlled trial evaluating the beneficial effects of yoga on 114 patients with migraines has shown a significantly greater improvement in various migraine measures, including headache frequency, intensity, and use of rescue medications [49]. Another randomized controlled study with 19 subjects suffering from episodic migraine has shown a reduction in headache intensity, duration, depression, and anxiety as well as an improvement of self-efficacy, migraine-related disability, and quality of life from baseline to initial follow-up[50]. A significant improvement of self-perceived pain frequency, pain intensity and duration, and psychological status as well as a reduction in medication consumption was observed in 31 patients with chronic migraine [51]. Furthermore, a significant decrease in headache frequency, medication intake, and stress perception has been reported in 20 patients with migraine or tension headaches [52]. Yoga has been suggested as a potentially effective approach to reducing headaches associated with menopause [53]. Multiple investigations have explored the mechanisms of action of yoga on headaches. Migraine is a neurovascular disorder with significant upregulation of endothelial adhesion molecules [2,54]. It has been suggested that yoga intervention alleviates pain primarily via modulation of the pain perception system, including the anterior cingulate cortex, insula, sensory cortex, and thalamus [55]. A study on 42 women with migraines evaluated the effect of yoga on endothelial dysfunction in migraine patients.
A 12 wk yoga training program increased delivering O2 to the body and reduced peripheral vascular resistance with a significant reduction in plasma values of vascular cell adhesion molecule, which suggests an improvement of vascular function in patients with migraine [8,51,56,57]. The amplitude of the contingent negative variation, an ultra-slow neocortical event-related potential, is significantly greater in patients with migraine compared to healthy controls, which indicates higher cortical excitability [58]. Subjects with migraines, who practice meditation, including yoga, have shown significantly lower amplitude of contingent negative variation [59].
Yoga and Alzheimer’s disease: Alzheimer’s disease (AD) is characterized by neuronal loss, mostly in the neocortex and the hippocampus [2,60], and is associated with memory and cognitive impairments and neuropsychiatric dysfunctions [2,60]. It has been suggested that yoga exerts a beneficial impact on overall brain health in healthy elderly subjects, older people with mild cognitive dysfunction, and subjects with dementia [61]. Yoga practice promotes cognitive function, affective interaction, and physical abilities of the healthy elderly population [62] and exerts a positive impact on total brain volume, neocortical grey matter thickness, and functional connectivity between different brain regions in subjects with mild cognitive dysfunction [63]. Using magnetic resonance imaging volumetric analysis, a trend toward decreased hippocampal volume atrophy has been observed after an 8 wk of yoga practice in patients with mild cognitive dysfunction [64].
A randomized neuroimaging study with 14 subjects has shown that yoga and mindfulness meditation may decrease hippocampal atrophy and promote functional connectivity between different brain regions, including the posterior cingulate cortex, the medial prefrontal cortex, and the hippocampus in adults susceptible to dementia [64]. Furthermore, it has been shown that mind-body interventions, such as yoga, can restore cognition in persons with mild cognitive impairment and delay the onset of AD [65,66]. Elderly subjects suffering from mild to moderate dementia have exhibited an improvement of behavioral impairments after a 12 wk yoga training program [67].
Metabolic enhancement for neurodegeneration, a novel therapeutic approach for AD, has merged yoga and meditation into other treatments of early AD pathology and achieved sustained cognitive improvement in 90% of patients [68]. Yoga may enhance blood flow to areas of the brain that modulate memory functions, reduce neuronal injury, promote the symptoms of early dementia, and delay the onset of AD [69]. Yoga can also improve the physical disability of patients with AD, such as walking, gait speed, and balance [70]. Although the mechanism of yoga action on AD needs to be elucidated, some possible mechanisms have been suggested. The serum values of several neurotrophic factors, such as brain-derived neurotrophic factor, increase after yoga practice in healthy individuals [71]. This may also occur in patients with mild to moderate AD and exerts a neuroprotective effect on the neurodegenerative process of AD [61]. The long-term practice of yoga also increases the serum value of serotonin [72]. The neuroprotective effects of yoga may be due to the enhancement of serotonin. Serotonin significantly destabilizes Aβ fibrils and protects neuron Aβ-induced cell injury and death [73]. The serum levels of melatonin significantly increased after a 3 mo period of yogic practices [74]. Melatonin reduces the Aβ level [75] and promotes micro vessel abnormalities in the neocortex and the hippocampus [76] in experimental AD models.
Yoga and epilepsy: The goal of therapeutic approaches for epilepsy, a common neurological disorder characterized by abnormal electrical brain activity [77], is to eliminate or decrease the number and duration of seizures and improve the quality of life [2,78]. Several studies suggest that yogic practices can ameliorate seizures in patients with different types of epilepsy. An investigation on the effects of yoga intervention on seizures and EEG of 32 patients suffering from idiopathic epilepsy has revealed 62% and 83% reduction of seizure frequency 3 and 6 mo after the intervention, respectively. Furthermore, this study has shown a significant shift of EEG frequency from 0-8 Hz toward 8-20Hz [79].
Another randomized controlled trial conducted on 20 children aged 8-12 years with epilepsy has suggested that a 6 mo yoga intervention as an additional therapy in children with epilepsy may lead to seizure freedom and a significant improvement of epileptiform EEG signals [[80]. The evaluation of the effect of yoga on clinical outcomes of 300 patients with epilepsy has suggested that yoga is a helpful approach for patients to manage their disease [71]. Contrary to these reports, a clinical study reported no significant differences between the frequency of seizures between the yoga and control groups. Nonetheless, the yoga group showed significant improvements in their quality of life [81]. An analysis of the data of two clinical trials that evaluated the effect of yoga on 50 epileptic patients suggests a possible beneficial effect of yoga in the control of seizures [82].
Yoga and multiple sclerosis: Several clinical trials investigated the potential beneficial effects of yoga therapy in patients with multiple sclerosis (MS), an autoimmune neuro inflammatory demyelinating disorder of the central nervous system [83]. A study tested the effects of a 6 mo yoga intervention on the improvement of different aspects of physical as well as psychosocial conditions in 44 patients with MS and 17 healthy relatives. This investigation has shown significant improvements in the quality of life, walking speed, fatigue, and depression values. However, yoga did not promote the pain, balance, and physical status of these patients [84]. A pilot study on 12 patients suffering from MS has suggested that various yoga training for 6 mo may lead to a significant improvement in postural balance and daily physical activities [85]. Another clinical study on 24 participants diagnosed with mild to moderate MS, which underwent an intensive yoga practice for more than 4 mo, has shown marked improvements in the peak expiratory flow rate, physical conditions, mental health, and quality of life of patients with MS [86]. A study conducted on 60 female patients with MS revealed that yoga training significantly improved physical abilities and sexual satisfaction [87]. Yogic training and relaxation have also been suggested for the improvement of neurogenic bladder dysfunction in patients with MS [88].
A qualitative case investigation on a woman with MS suggested that individualized yoga intervention for 6 mo could be beneficial for the improvement of muscle tone and strength as well as self-confidence and stamina [89]. A significant improvement in balance, gait, fatigue, walking speed, and step length has been reported in 18 patients with relapsing-remitting MS after a 12-wk yoga training [90]. Yoga intervention has also exerted a beneficial role on improvements of postural balance and reduction of the influence of postural balance impairment during daily activities in patients diagnosed with MS after yoga practice for 6 mo[85]. A meta-analysis of 10 randomized controlled trials with overall 693 patients with MS who trained with different forms of yoga has revealed a significant improvement of fatigue but no effects on the overall quality of life, sexual function, and psychosocial condition [91].
Yoga and Parkinson’s disease: The potential beneficial therapeutic effects of a yoga intervention for Parkinson’s disease (PD), a chronic and debilitating neurodegenerative disorder, have been investigated. Yoga exerts a range of beneficial effects on different symptoms of PD [[92]. A question-based survey on 272 patients with PD has shown that the majority of patients found yoga and meditation helpful for the alleviation of both motor and non-motor (fatigue, sleep difficulties, pain symptoms [93]. A randomized clinical study on 126 patients with mild to moderate PD who underwent weekly yoga training for 8 consecutive weeks has shown a significant alleviation of psychological symptoms, improvement of the quality of life, and reduction of motor symptoms [94]. Yoga exercises can improve flexibility and balance, decrease muscle rigidity, increase the range of motion, and promote muscle strength in patients with PD [[95]. Yoga intervention effectively improves balance and proprioceptive acuity in 33 patients with mild to moderate PD [96]. It has been suggested that incorporating yoga and occupational therapy may promote balance and decrease falls in patients with PD [97]. Yoga training decreases the back pain associated with a lower postural instability, which may reduce falls in patients with PD [98]. Furthermore, yoga as adjunctive therapy in patients with PD has been suggested as an effective treatment for the reduction of psychological complications, particularly anxiety and depression [99-101].
Yoga and neuropathy: Peripheral neuropathy is a common neurological condition due to physical nerve injury, diabetes mellitus, autoimmune disorders, malignancy, kidney failure, nutritional deficiencies, systemic disorders, and idiopathic neuropathies, which can implicate the motor, sensory, and/or autonomous peripheral nerves [102,103]. Several lines of evidence suggest that yoga may alleviate symptoms of various neuropathies [104,105]. Several reports suggest the beneficial effects of yoga practices in patients with neuropathy. Yoga practices were shown to improve numbness and weakness in lower extremities after a stretch or compression injury of the gluteal nerves [106], alleviate chronic pain due to diabetic neuropathy [107], and promote sensory functions and muscle movement in subjects with diabetic peripheral neuropathy [108]. However, it should be noted that some reports indicate yoga-induced nerve injury and neuropathy [109-111], particularly in patients who take sedative medications, people with benign hypermobility of their connective tissue, and the elderly [110,112,113]. Furthermore, yoga may ease compression and decrease nerve compression in carpal tunnel syndrome, which could lead to the improvement of numbness after a few weeks of practice [114,115]. Yoga meditation therapy improved the nerve conduction velocity, which was associated with glycemic control, in patients with diabetic neuropathy [116,117]. A reduction of the impact of chemotherapy-induced peripheral neuropathy symptoms on the lives of patients with breast cancer as well as on the pain intensity after yoga intervention has been reported [118,119].
The Clinical Role of Yoga in Psychological Disorders
Yoga, stress, and anxiety: Stress and anxiety are increasing in incidence worldwide. Approximately 34% of the general population is affected by an anxiety disorder during their lifetime [120]. Several investigations were performed on the feasibility and potential efficacy of different forms of yoga on anxiety- and stress-induced symptoms in both children and adults. It has been suggested that yoga may promote mental and physical strength, increase stress resilience, and reduce anxiety [121]. Although some studies do not show any effect [122,123], most investigations indicate that yoga can be effective in the alleviation of anxiety in the form of monotherapy or adjunctive therapy [124-127]. Functional magnetic resonance imaging evaluation revealed that yoga interventions modulate the activity of various brain areas that are crucial to emotion regulation, such as the superior parietal lobule and supramarginal gyrus, and lead to a diminished sympathetic response to stressful emotional stimulations [128]. Training of mindfulness- and yoga-based programs has shown a significant reduction of anxiety symptoms, which was associated with a marked decrease of structural connectivity of the right amygdala [129]. Furthermore, it has been suggested that yoga intervention modulates stress-induced autonomic regulatory reflex and inhibits the production of adrenocorticotropic hormone from the anterior pituitary gland [130], resulting in decreased production of cortisol from the adrenal gland [131].
A meta-analysis revealed that more yoga exercises were accompanied by greater benefits, particularly when subjects were suffering from higher values of anxiety at the early stages [132]. Another meta-analysis of eight trials with 319 adults diagnosed with anxiety disorders who underwent yoga training indicates that yoga could be a safe and effective intervention to reduce the intensity of anxiety [133]. Rhythmic yoga meditative interventions resulted in a reduction of stress associated with a higher plasma dopamine level together in 67 healthy subjects who regularly engaged in mind-body training [134]. Enhancement of dopamine values following yoga practice leads to a suppression of corticostriatal glutamatergic transmission and regulation of conscious states [29]. Yoga interventions have been suggested to enhance vigilance, improve sleep, and reduce anxiety in healthy security personnel [135].
Yoga-based exercises in schools have been suggested to reduce stress and challenging behavioral and cognitive responses to stress, promote physical ability, and strengthen cognitive performance among students [136,137]. Yoga interventions for a period of 8 wk have shown a significant impact on reducing anxiety in school-age children [138]. Using a yoga-based relaxation method (mind-sound resonance technique) alleviated state anxiety and mind wandering and promoted state mindfulness and performance in school children [139]. High-frequency yoga breathing training promotes attention and reduces anxiety in students aged 11-12 years [140]. Furthermore, evaluation of the effect of yoga intervention on stress perception and anxiety levels in college students has shown a significant reduction in anxiety and stress scores associated with a marked enhancement of total mindfulness [141]. Yoga can also help adolescents hospitalized in an acute care psychiatric ward to lessen their emotional distress [142]. Yoga exerts a bifacial effect on the reduction of anxiety and improvement of self-esteem in orphanage residents [143].
Practicing yoga in patients suffering from post-traumatic stress disorder for at least 4 wk resulted in a significant reduction of cortisol values [144]. Yoga practices significantly reduce stress and anxiety in subjects living with human immunodeficiency virus [145], people with cancer [146], such as survivors of lung cancer [147] and patients with breast cancer [148], patients with systemic disease, like rheumatoid arthritis [149,150], and patients with neurologic disorders, such as PD [100]. Yoga exercises have also been suggested as a promising stress-relieving approach in pregnant women [151,152], in women receiving treatment for infertility [153], and in women who are trying to quit smoking [154,155].
Yoga and depression: Depression is the most common psychiatric disorder that affects 25% of women and 12% of men during their lifetime [156-159]. This disorder is commonly treated by antidepressants and psychotherapy [156,160]. Yoga interventions have been suggested as effective adjuvant therapy [161,162] as well as monotherapy [163] for depression.
A narrative review on the efficacy of yoga and mindfulness as an adjuvant treatment in severe mental illnesses including major depressive disorder (MDD) indicated that both yoga and mindfulness have significant and beneficial effects on reducing the severity of depressive symptoms [164]. Yoga practices in combination with the application of conventional antidepressants significantly improved depression symptoms and reduced the remission rate in patients with MDD compared to control patients [165]. A significant decrease in self-reported symptoms of depression after practicing yoga has been observed in individuals aged 18-29 with mild levels of depression [166]. A meta-analysis has shown a more significant reduction in depression compared to psychoeducation [167].
In addition to the improvement of depression, yoga interventions promote mental health and quality of life and interrupt negative thinking in patients with depression [168,169]. A meta-analysis of 10 studies has shown that yoga practices have a statistically significant effect as an adjunct treatment in patients with MDD [162]. In an investigation of hospitalized patients with severe MDD, the effect of yoga intervention was equivalent to treatment with a tricyclic antidepressant [170]. It has been suggested that yoga modulates cortical inhibition via the regulation of the GABAergic system and exerts beneficial effects in MDD [171]. Furthermore, increased GABA-mediated neurotransmitter activity induced by transcranial magnetic stimulation, and multiple yoga therapy sessions was associated with a significant improvement of depression symptoms in patients with MDD [172]. Enhancement of thalamic GABA values has also been suggested as a potential mechanism for the improvement of mood in patients with MDD [173]. Enhancement of serum neurotrophic factors, such as brain-derived neurotrophic factor, in patients with MDD who practiced yoga, pointed to the possible role of increased neuroplasticity in the improvement of depression symptoms [174]. Yoga practices in post-menopausal women resulted in reduced values of follicle-stimulating hormone and luteinizing hormone, which was associated with decreased stress levels and depression symptoms as well as improved quality of life [175]. Yoga practices in association with coherent breathing intervention have been shown to resolve suicidal ideation in patients with MDD [9,176].
Yoga and bipolar affective disorder: Bipolar affective disorder (BD) is a chronic illness with recurrent episodes of manic-depressive symptoms [177,178]. Although most patients with BD are free of symptoms during remission, many of them continue to experience mild symptoms and suffer from functional behavior impairments [177,179]. Studies on the role of yoga in the treatment of BD are scarce. However, some studies have recommended yoga as a specific self-management strategy for BD [[5,180]. Patients with BD have shown a significant alleviation of depression and anxiety symptoms, reduction in difficulties with emotion regulation, and improvement of mindfulness skills during the remission phase following several weeks of yoga practices [181]. Yoga interventions have been suggested to decrease negative emotions in patients with BD [[182]. Yoga has also been suggested as an adjuvant therapy that improves residual depression symptoms [183] as well as manic symptom severity [184] of patients with BD. An extensive multicenter, randomized controlled study on 160 adults with BD has shown that mindfulness-based cognitive therapy, including yoga practices, improves the severity of manic symptoms and anxiety, promotes mental health and overall functioning, and reduces relapse rates [185].
Yoga and schizophrenia: Schizophrenia (SZ) is a severe mental disorder, which often exhibits itself by positive symptoms, including hallucinatory experiences and delusional beliefs and negative symptoms, such as lack of motivation and social contacts as well as the absence of spontaneous speech and affective flattening [186-188]. A growing body of evidence suggests that yoga training as an add-on therapy could improve both the negative and positive symptoms and promote cognitive functions and emotional recognition of SZ [189-194].
The analysis of yoga intervention effects on the mood of 113 patients with psychosis has revealed significant improvements in tension-anxiety, depression, anger, fatigue, and confusion [195]. Another study on 66 antipsychotic-stabilized patients with SZ has revealed a significant improvement in positive and negative symptoms, socio-occupational functioning, and performance following yoga training [190]. A meta-analysis of 13 investigations with 1159 patients revealed the importance of the frequency of yoga interventions with an improvement of positive symptoms as well as the duration of each session with the alleviation of negative symptoms in patients with SZ [196]. Yoga practices in the patients with SZ who were taking antipsychotic medications and were in a stable condition significantly decreased drug-induced parkinsonian symptoms and improved executive functions and negative symptoms [192]. Long-term yoga intervention in patients with SZ resulted in greater social and occupational functioning and promoted the quality of life [197]. Yoga training in patients with SZ resulted in an improvement of negative and positive symptoms associated with a reduction of paranoid beliefs and promoting quality of life [198]. Yoga as an add-on treatment has shown a greater improvement of the negative symptoms of SZ in comparison to physical exercise therapy [197]. Furthermore, yoga therapy led to a significant reduction in burden scores and an improvement in the quality of life among patients with psychosis [199]. Yoga intervention in patients with SZ significantly improved cognitive dysfunction, presumably through the correction of autonomic dysfunction [200,201].
It has been suggested that yoga may improve SZ symptoms by strengthening the synaptic network of the lateral and medial prefrontal areas and augmentation of the premotor and parietal mirror neuron circuitry [202]. Oxytocin values increased significantly following yoga practice [203]; an effect that has been suggested to play a potential role in the improvement of social cognition after yoga intervention in patients with SZ [204]. Yoga practice in patients with SZ was also associated with a significant decrease in blood cortisol levels, suggesting a beneficial effect of yoga in the reduction of social physical stress of patients [204].
Yoga and other psychological disorders: Several other studies indicate the potential beneficial effects of yoga practices on other psychological disorders and syndromes, such as obsessive-compulsive disorder (OCD), burnout, somatoform disorders, and hypochondriasis [[205]. The treatment of OCD with yoga together with the pharmacological interventions improved the obsessive thoughts and compulsive behavior of patients with OCD [[206,207]. Furthermore, several clinical trials have suggested the promise of yoga intervention as an adjunct therapy for patients with OCD, who were unresponsive to conventional treatments [208,209]. Moreover, yoga training enhanced general satisfaction, improved work exhaustion, and led to greater work engagement and empathy among teachers [21], nurses [211], hospice professionals [212], and physicians [213,214], who were suffering from job burnout. Yoga can promote the psychological and physical well-being of subjects with burnout, particularly when combining it with other activities, such as art and music-therapy [215,216]. Furthermore, yoga-based interventions have been recommended as an effective therapeutic approach in somatoform disorders [217]. A 6 mo trial of yoga practices led to a significant improvement of somatoform symptoms, such as gastrointestinal, cardiovascular, and urogenital symptoms, in women with the menstrual disorder [218]. Several studies have revealed the beneficial effects of yoga interventions on the psychological health of the population during the global pandemic of coronavirus disease 2019 [219].
ADVERSE EFFECTS OF YOGA
The musculoskeletal complications, including back, shoulder, or neck pain, osteoarthritis, joint injuries and dislocations, fractures, disc herniation, and tendon deformities have been reported as common adverse effects of yoga practice [221-223]. However, the frequency of severe injuries associated with yoga is low (less than 5%), and both acute and chronic injuries recover fully [224,225]. Moreover, there are several reports of peripheral nerve injuries after a yoga practice, particularly in the elderly subjects who take sedative medications and patients with hypermobility of the connective tissue [104-106].
CONCLUSION
Most scientific publications on yoga deal with the efficacy of said programs to gain an understanding of the subject to counsel patients appropriately. However, the usefulness of meditation specifically for clinicians, as an occupation group that is particularly associated with physical and mental health risks, still needs more accurate evidence. Although most investigations are in favor of the beneficial effects of yoga on neuropsychological disorders, some studies have not found this meditative procedure useful. Several points in the studies that have shown the beneficial impacts of yoga on neuropsychological disorders have to be taken into consideration. Multiple investigations reporting beneficial effects of yoga on neuropsychological disorders were not precise in design, implementation, and analysis. There was considerable heterogeneity among the description of yoga interventions in different studies. Different yoga types and many disciplines within the practice have been conducted with various duration and frequency of training. Differences in yoga approaches and the use of different outcome measurements may explain why the outcome of yoga interventions often differed in patients with a common pathological circumstance. Furthermore, many of these studies have several limitations, such as small sample sizes, short-term follow-up, confounding variables, and lack of appropriate controls. The heterogeneity of intervention procedures and poor qualities of the original investigations substantially influence the value of the meta-analyses that evaluated the effects of yoga on various disorders. Several studies evaluated the underlying mechanism of action of yoga on neuropsychological disorders. However, the exact mechanisms remain to be further elucidated. Although yoga is a complex approach and difficult to standardize, it is crucial to distinctly describe the intervention procedures, both conceptually and operationally, and avoid excessive heterogeneity [226,227] to consider them as an integrative method in treatment plans for neuropsychological disorders [228]. Furthermore, accurate selection of populations and controls is of great importance to evaluate the potential benefit of yoga on patients with neuropsychological diseases.
References
Elnaz Nourollahimoghadam, Shefa Neuroscience Research Center, Khatam Alanbia Hospital, Tehran 1996835911, Iran
Shaghayegh Gorji, Ali Gorji, Epilepsy Research Center, Münster University, Münster 48149, Germany
Ali Gorji, Department of Neuroscience, Mashhad University of Medical Sciences, Mashhad 9177948564, Iran
Maryam Khaleghi Ghadiri, Department of Neurosurgery, Münster University, Münster 48149, Germany
See here (wjgnet.com) for a full list of each reference in the article.
Nourollahimoghadam E, Gorji S, Gorji A, Khaleghi Ghadiri M. Therapeutic role of yoga in neuropsychological disorders. World J Psychiatr 2021; 11(10): 754-773 [PMID: 34733640 DOI: 10.5498/wjp.v11.i10.754]